Other autoimmune diseases
1. Circulating Immune Complexes (CIC) and Complement System
The complement system is an important part of the immune system with a number of biological effects that mainly contribute to an inflammatory response and thus to the activation of cells such as leukocytes and endothelial cells. An intact complement system is essential for protection against infection. Nevertheless, this system is a double-edged sword: increased, uncontrolled or incorrect activation can potentially be dangerous to the patient.
Complement activity plays an important role in the pathogenesis of systemic autoimmune diseases.
Activation takes place via 3 ways:
- Classic way
- Binding of an antibody to an antigen
- Lectin way
- Mannose binding lectin (MBL)
- Via certain surface structures of bacteria
- Via certain IgA forms
- Via damaged endothelium
- Alternative way
- Is not activated directly, but by spontaneous decay of C3 in C3a
C3b is always active at a low level
- Is not activated directly, but by spontaneous decay of C3 in C3a
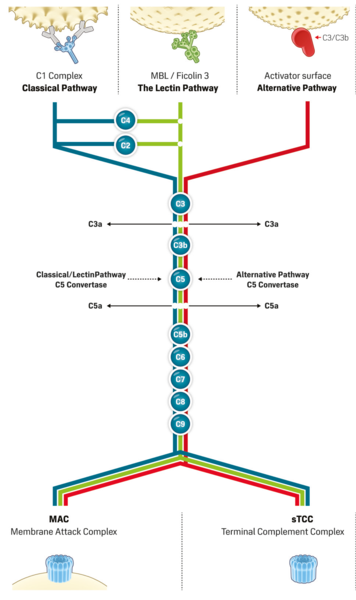
The essential functions can be summarized in 4 mechanisms:
- Opsonization of foreign cells, especially with C3 products
- Chemotaxis by C5a release and subsequently phagocytosis of the pathogen
- Lysis by Pore Formation in the Membrane (C5b-9)
- Immune system regulation
However, the complement system is also activated by circulating immune complexes (CIC) in the bloodstream. These circulating immune complexes (CIC) are aggregates (aggregations) of antibodies and structures dissolved in the blood against which these antibodies are directed (antigen - antibody complexes).
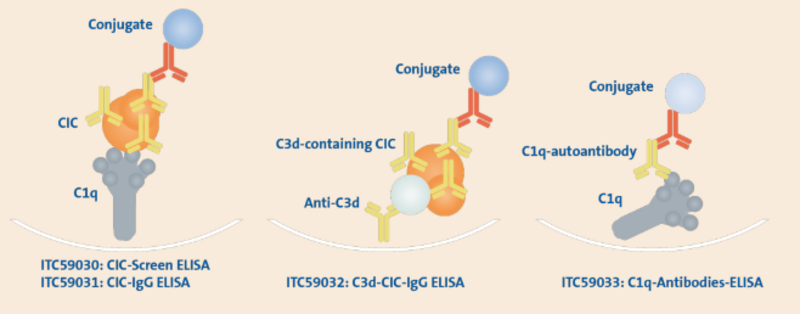
Normally, immune complexes are taken up by phagocytes or macrophages immediately after their formation. However, if too many immune complexes are produced, this exceeds the capacity of the phagocytes and the immune complexes can enter the blood in larger quantities.
In complement activation, fission products such as C3d can be detected in patients with lupus nephritis or in patients with cutaneous systemic scleroderma.
There are different types of immune complexes depending on which antibodies and antigens are included:
- immune complexes with antibodies of the type IgG, IgA, IgM
- Immune complexes with complement factors (C1q, C3c, etc.)
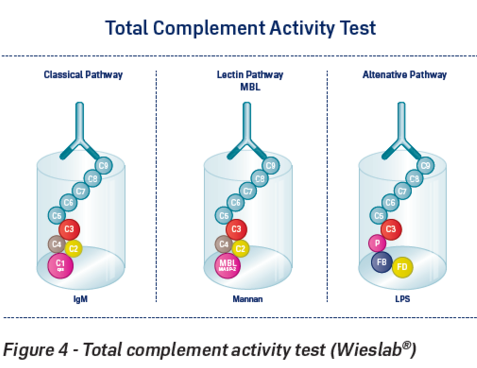
Determination of CIC and complement system
- CIC IgG / IgM
- C3d - CIC
- Complement system Screen (alternative, classical and MBL pathway)
- Complement system alternative way
- Complement system Classic way
- Complement system MBL way
2. Chromogranin A (CgA)
Tumors of neuroendocrine origin, such as carcinoids, typically have elevated levels of chromium organine A in serum and plasma.
There are other causes for elevated Chromogranin A, but in the presence of neuroendocirne tumors, monitoring Chromogranin A levels can be helpful in assessing the efficacy of treatment.
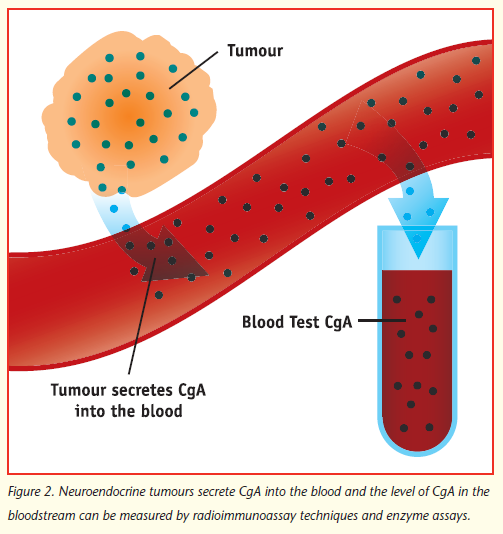
Chromogranin A has been detected in a variety of neoplastic tissues (especially neuroendorkin origin):
- Small cell bronchial carcinoma
- Insulinom
- Neuroblastoma
- Medullary thyroid carcinoma
- Pheochromocytoma
An increase in chromogranin A is also found in some non-malignant diseases:
- Chronic gastritis
- Inflammatory bowel disease
- Heart failure
- Rheumatoid Arthritis
- ...
Determination of Chromogranin A
- Chromogranin A ELISA

 Deutsch
Deutsch


